Program Features
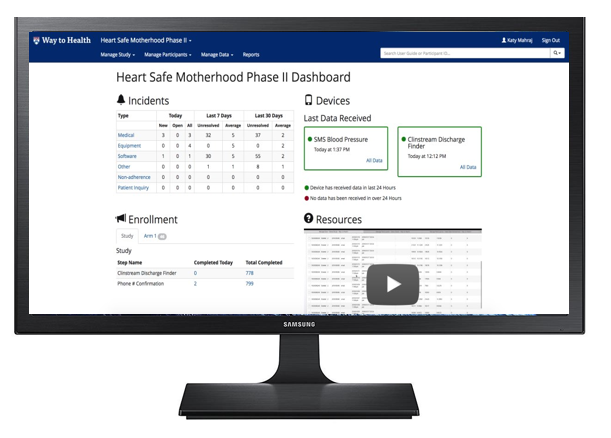
Heart Safe Motherhood is an evidence-based approach to patient identification, engagement, and early intervention powered by a bi-directional, text message-based platform. The platform, called Way to Health, generates automated, real-time feedback to patient-reported blood pressure readings and alerts providers to values that require intervention.
The program, which is administered and managed through Way to Health, enables patients to track their blood pressure from the comfort of their homes and communicate with their care team without visiting a doctor's office.
Inpatient clinicians on labor and delivery and postpartum service identify and enroll at-risk women in the program based on eligibility criteria, including diagnoses and vital signs. From there, participants are given a digital blood pressure monitor for at-home use. Training on how to use the monitor and education about the program also occurs before discharge.
Upon discharge, an automated blood pressure monitoring protocol is enacted. Patients are prompted twice daily via text message to take their blood pressure and share it with their care team. Patients with blood pressures within the normal range receive automated, real-time feedback based on a provider-determined algorithm. And when blood pressures are high enough to necessitate intervention, HSM pushes real-time alerts to providers so that, depending on the circumstances, they can reach out for more information, start or adjust medication, or triage patients to in-person care.
Through automation and exception handling, HSM makes it possible for one provider to manage the blood pressures of an entire hospital's worth of enrolled deliveries in just a few hours a week.
The program provides at-risk women with high quality, convenient care outside the traditional boundaries and habits of health systems, driving better maternal outcomes, improving patient experience, and reducing the cost of care for women with pregnancy-related and chronic hypertension during a woman’s transition home from the hospital after delivery. To date, we have demonstrated significant improvement in our ability to obtain blood pressure readings at the two recommended time points to consistently over 80% and a reduction in seven-day postpartum readmissions for hypertension by 80%.
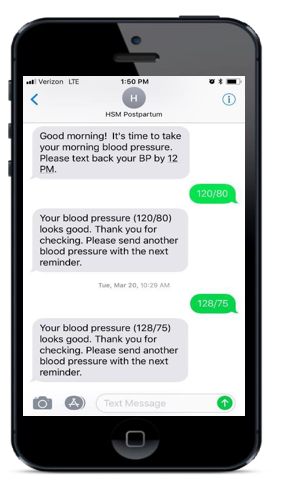
On the day after discharge, patients start on a remote monitoring protocol with automated reminders and feedback over a ten-day surveillance period enabled by Way to Health, a Penn-developed platform for evidence-based, personalized engagement strategies.
Efficient automationProviders focus on the information they need to know through alerts and dashboards. Providers are alerted only when blood pressures are high enough to necessitate intervention.
Real-world expertiseThe Heart Safe Motherhood approach to patient identification, education, engagement, monitoring, and management was developed over four years to maximize impact, convenience, ease of use, and patient safety.
Continual innovationHeart Safe Motherhood is continuously evolving as we find new ways to engage patients, improve provider experience, and maximize impact through real-world implementations and innovative research.
