The Evidence
Evidence from the Randomized Trial
In 2017, we completed a randomized controlled trial comparing Heart Safe Motherhood to the usual care of one-time, office-based blood pressure checks. We found an increase in our ability to obtain at least one blood pressure within ten days after discharge, with 92% of patients texting a blood pressure compared to 44% office visit attendance. We met American College of Obstetrician and Gynecologists (ACOG) guidelines for blood pressure ascertainment at the two recommended time points (72 hours and 7-10 days postpartum) in 80% of patients.
There were no readmissions among text-message based monitored women, and women enrolled in the program were more likely to attend their postpartum visit. Results were published in BMJ Quality and Safety.
Given the promising findings, we scaled HSM to HUP in 2017, PAH in 2018, and Princeton in 2019. At the time, we had enrolled over 4,000 postpartum women from the three Penn Medicine hospitals, obtaining over 50,000 blood pressures. We have consistently obtained blood pressures at the ACOG recommended time points in over 80% of our patients and start medications remotely in about 15% of enrolled women.
We continue to have strong patient and provider satisfaction. Postpartum hypertension readmission rates at HUP dropped from 5% prior to HSM to 1% with the program at scale. Hypertension is no longer the leading cause of seven-day obstetrical readmissions at HUP. Unpublished quality improvement work since scaling efforts at Pennsylvania Hospital and Princeton Medical Center show similar rates of blood pressure ascertainment, at over 90% at both hospitals, and readmission rates for postpartum hypertension closer to 2%.
Eliminating Disparities
A planned secondary analysis of the trial found that our program eliminated the observed racial disparities in postpartum hypertension care. Prior to the intervention, non-black women were significantly more likely to attend an in-person blood pressure check than black women, yet black women were at higher risk of poor outcomes. With HSM, we were able to increase our ability to capture blood pressure for all patients while also eliminating the racial disparities previously observed. Results were published in the American Journal of Obstetrics and Gynecology.
Reduction in Long-Term Adverse Events & Cost Savings
We published a study with IBX, Association of a Remote Blood Pressure Monitoring Program With Postpartum Adverse Outcomes, to evaluate the association of a text-message based remote BP monitoring program with adverse postpartum clinical outcomes and costs in patients with hypertensive disorder of pregnancy.
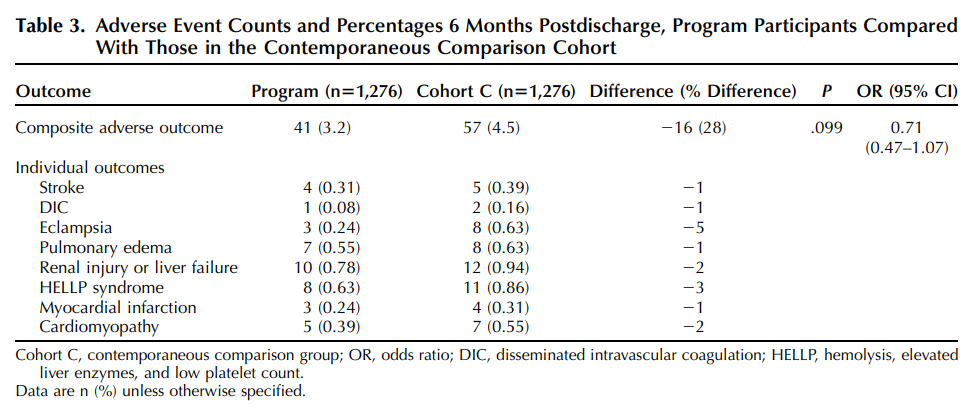
It was found patients enrolled in HSM were less likely to experience an adverse clinical outcome in the first 6 months after delivery, compared with patients in either comparison cohort. Program participants had reduced ED visits and readmissions resulting in lower postpartum total medical costs compared with both comparison cohorts.
We continued to conduct an administrative claims data analysis showing long-term postpartum clinical and cost outcomes related to a remote monitoring program for postpartum hypertension. It revealed that the positive outcomes persisted over 12 months.
For a more in-depth discussion, we collaborated with Obstetrics & Gynecology on a podcast episode - listen here!
